For most metastatic cancer types, there are no reliably effective treatments. Therapies may slow the growth of tumors, but they will not eradicate them. Occasionally, however, treating a tumor in one location will cause untreated tumors elsewhere in the body to shrink or even regress completely — a dramatic but exceedingly rare phenomenon known as the abscopal effect.
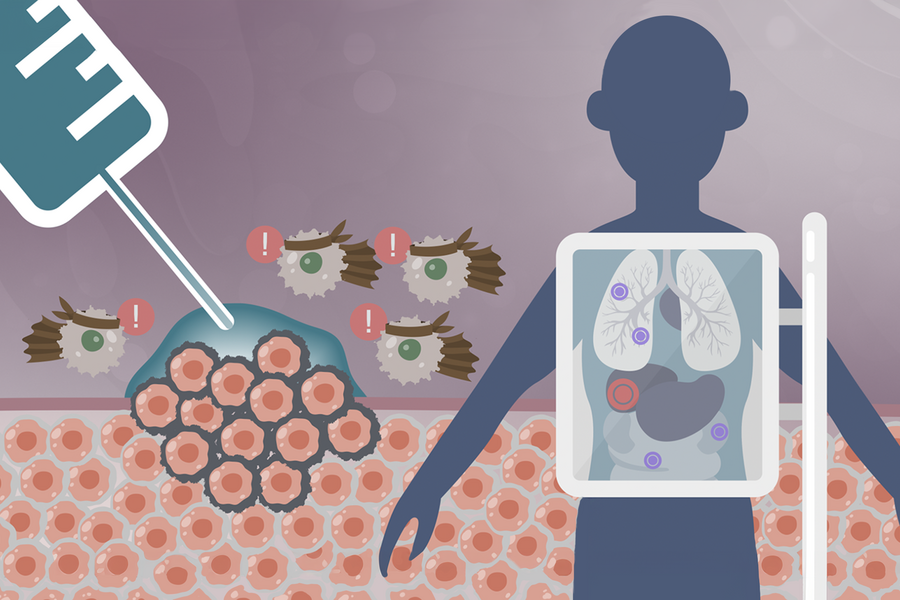
Cancer researchers have sought methods to induce the abscopal effect by design. The abscopal effect is thought to arise when dead or damaged tumor cells release antigens that teach some types of immune cells to recognize and attack other and even distant cancer cells. Essentially, the treated tumor behaves like a personalized cancer vaccine that incites the immune system to attack metastasized tumors. The advent of cancer immunoadjuvants, which enhance and sustain the activity of tumor-targeting immune cells, has been a key to unlocking the abscopal effect, at least in the laboratory setting.
In the clinic, success has proven more elusive. Since immunotherapies can lead to serious toxicities if administered through the bloodstream, they must be delivered directly to the tumor — often by injection. It is difficult for clinicians to target injections precisely to the tumor and impossible to confirm delivery. Once injected, immunostimulatory drugs quickly leak out of the tumor before they have had a chance to take full effect.
MIT researchers, together with colleagues from Mass General Brigham, have developed a polymer gel delivery system that could help translate the promise of the abscopal effect into the clinic. The gel, visible with a CT scanner or ultrasound, solidifies after injection, where it remains in the tumor to release drugs at a controlled rate.
In a study published in Advanced Healthcare Materials, the team delivered the immune-stimulating drug imiquimod in combination with checkpoint blockade therapy to dual-tumor mouse models of colon and breast cancer, which showed improved survival as well as tumor regression in both treated and untreated tumors.