With CAR-T cell therapy, a patient’s own immune cells are harvested and genetically engineered to recognize a specific tumor antigen and attack cancer cells. Although CAR-T cell therapy has shown remarkable outcomes in certain blood cancers, it has struggled to succeed in solid tumors. The challenges include poor tumor penetration, toxic side effects, development of resistance mechanisms and the complex, patient-specific engineering process required for each treatment.
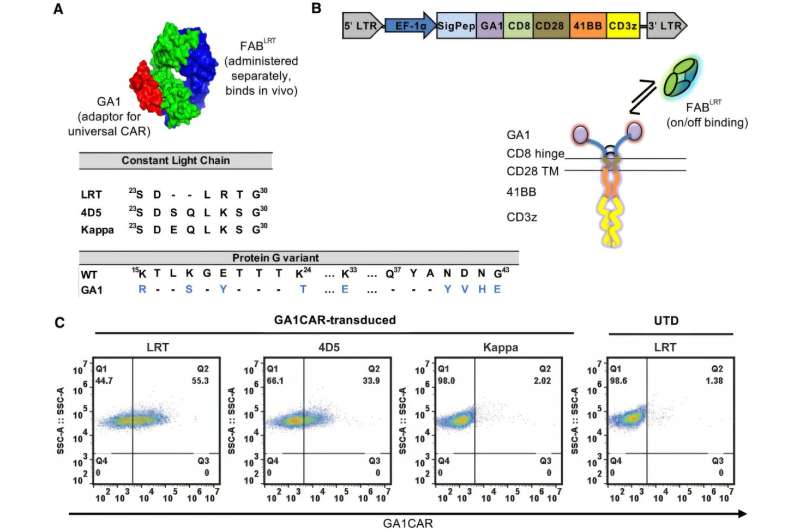
Traditional CAR-T cells rely on a fixed antigen-binding domain, which means they can only target one type of cancer antigen. A single CAR-T cell contains an antigen recognition unit attached to signaling machinery—making it a large construct that may contribute to toxicity. Moreover, tumors often display antigens in different degrees, and tumors may escape from CAR-T cell therapy by losing CAR-T targeted antigens.