The study is published in the journal Frontiers in Pharmacology.
Scaffolds are made of an engineered biomaterial that provides support for new tissue formation. Normal skin tissue contains skin cells and an extracellular matrix that harbors proteins and small molecules that help repair and nourish tissue. These cells and extracellular matrix elements are lost at large deep burn wound sites.
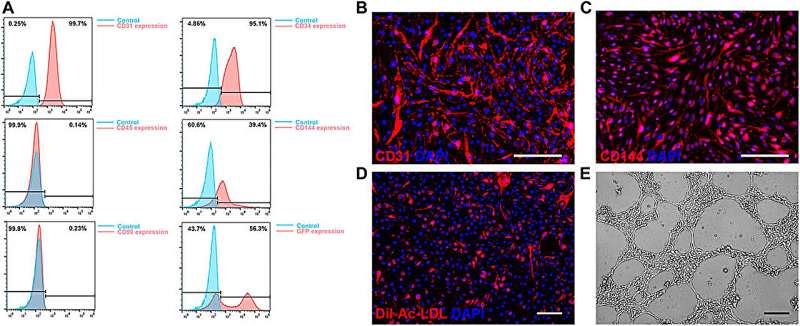
Wang and his team engineered a scaffold that is modified with a special molecule known as LXW7 that specifically interacts with endothelial cells to help the wounds heal.
“Endothelial cells play a critical role in the body’s homeostasis and regeneration. They help in blood vessel formation during wound healing and regulate the movement of substances across the body,” said Wang, professor of surgery and biomedical engineering. He is also the vice chair for translational research, innovation and entrepreneurship in the Department of Surgery and co-directs the Center for Surgical Bioengineering at UC Davis, and leads the Wang Lab.
“At UC Davis, we developed the LXW7 molecule that can specifically interact with endothelial cells and help in their attachment, migration and survival. Commonly used scaffolds lack specific binding sites to endothelial cells. When LXW7 molecules are added to scaffolds, they provide a gripping site for endothelial cells to bind, which allows for better interaction between the cells and their supportive structure known as extracellular matrix,” Wang explained.
In their study, the team showed that the engineered scaffold can accelerate wound healing in mice and lower the risk of burn complications, such as fluid losses and infection.
The study also indicated that the engineered new scaffold may reduce, or even remove, the need for autografting—the transplantation of the patient’s skin from one body part to the burn location. With the new scaffold, there is less risk of autografting complications, especially in patients with little skin that can be used for the procedure.